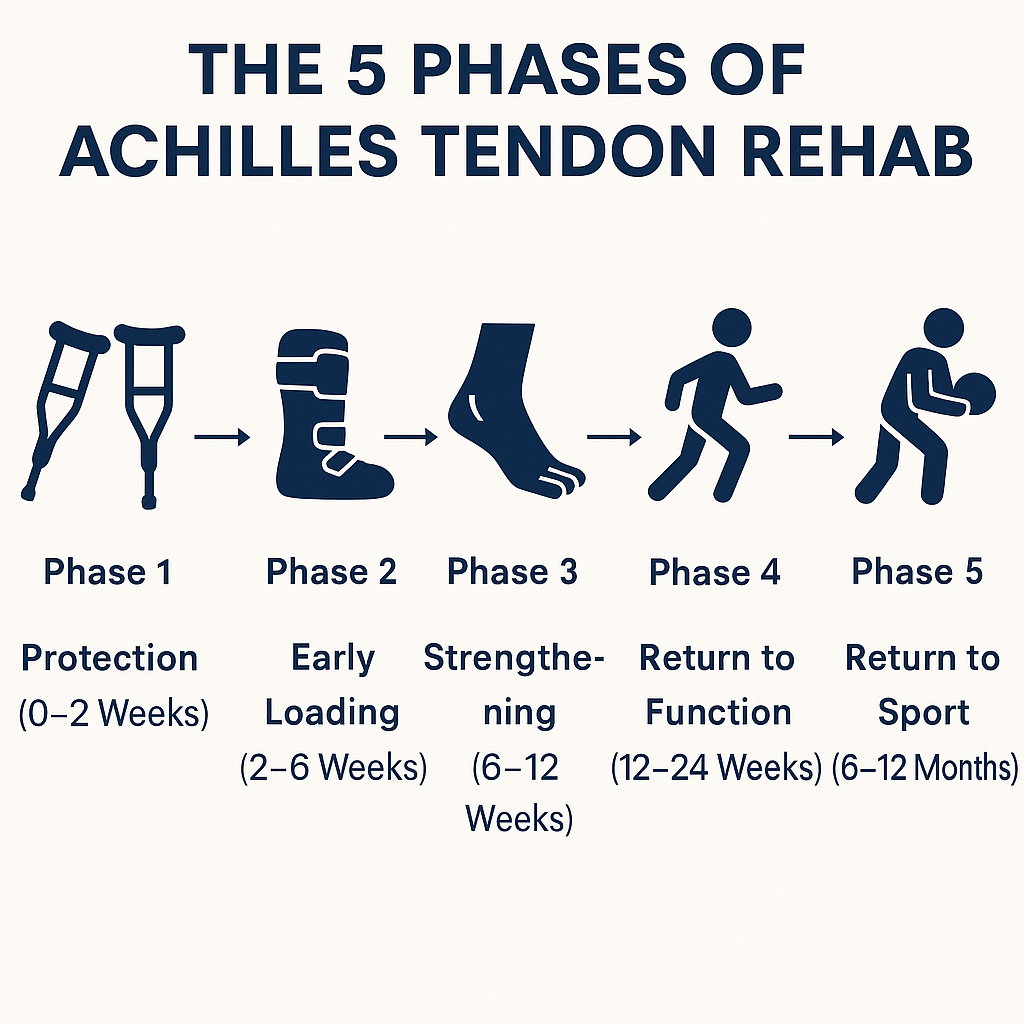
Learn the five key rehab phases after Achilles tendon repair in Hillsboro and Portland, from protection to sport-specific training
Introduction
An Achilles tendon rupture is one of the most serious injuries an athlete or active individual can face. Whether it happens during a basketball game in Beaverton, a run in Forest Park, or a soccer match in Hillsboro, the road back requires careful planning and structured rehabilitation.
Physical therapy after surgical repair is usually divided into phases. Each phase has unique goals, restrictions, and milestones. The goal isn’t just to heal—it’s to restore tendon strength, prevent elongation, and ensure a safe, confident return to activity. Below is a breakdown of the five phases, based on the latest clinical guidelines and evidence.
Phase 1: Protection (0–2 Weeks)
In the first two weeks, the tendon repair is at its most vulnerable. The focus is on:
-
- Protecting the repair with a cast or walking boot (often with heel wedges).
-
- Controlling swelling and pain through elevation, rest, and cryotherapy.
-
- Preventing complications like infection or deep vein thrombosis.
Patients in Portland clinics are typically non-weightbearing, using crutches or a scooter. Even in this early stage, therapy may include:
-
- Gentle hip and knee exercises to maintain strength.
-
- Isometric calf contractions inside the boot to stimulate blood flow.
-
- Blood Flow Restriction (BFR) training on the non-injured side or upper leg, if cleared by the surgeon.
The goal is simple: keep the rest of the body strong, manage swelling, and allow the tendon to begin its healing process without disruption.
Phase 2: Early Loading (2–6 Weeks)
This is the critical window where controlled loading begins. Research shows that early mobilization and weightbearing do not increase rerupture rates and may even improve tendon healing.
Key elements in this phase include:
-
- Partial weightbearing (PWB) in the walking boot, progressing toward full weightbearing (FWB) by week 4–6.
-
- Heel lifts inside the boot, reducing calf strain by up to 57% during walking.
-
- Active range of motion (AROM) up to neutral dorsiflexion (toes pointed straight), but avoiding stretching past neutral to prevent elongation.
-
- Sub-maximal isometric exercises in shortened calf positions.
During this time, therapists in Hillsboro or Beaverton emphasize walking with shorter strides and controlled gait mechanics. Patients may also begin low-impact cardio like a stationary bike once the incision heals.
Phase 3: Strengthening (6–12 Weeks)
By this stage, the tendon is stronger, and therapy shifts toward rebuilding power and control:
-
- Transitioning out of the boot into supportive shoes with heel lifts.
-
- Double-leg heel raises, gradually progressing to single-leg heel raises.
-
- Balance and proprioception drills, such as standing on one leg or using wobble boards.
-
- Gradual restoration of dorsiflexion ROM, always avoiding aggressive stretching.
Despite progress, strength deficits are still common—only about 50% of patients can perform a strong single-leg heel raise at 12 weeks. Therapists use tools like AlterG treadmills or aquatic therapy to unload body weight and build movement quality without risking overstress.
Phase 4: Return to Function (12–24 Weeks)
Now the rehab starts to feel more like athletic training. The focus is on preparing for sport-like demands:
-
- Jogging and low-level plyometrics (like pogo hops or band-assisted jumps) once strength benchmarks are met.
-
- Advanced strengthening through calf raises, squats, lunges, and resisted movements.
-
- Agility and movement drills, restoring the ability to cut, decelerate, and sprint.
Criteria for progression include:
-
- At least 10 strong single-leg heel raises.
-
- Strength symmetry within 70–80% of the uninjured side.
-
- Proper mechanics during walking and running drills.
This is also when therapists address the contralateral limb (the uninjured side), which often loses conditioning during recovery and is at risk of future injury.
Phase 5: Return to Sport (6–12 Months)
The final stage is about regaining full performance capacity. Return to sport is not just about time—it’s about meeting objective criteria:
-
- 90% limb symmetry in strength and hop testing.
-
- Seated calf strength of at least 1.5–2.0 times body weight.
-
- Controlled plyometrics with less than 20% asymmetry in jumps.
In Portland’s competitive leagues, basketball or soccer players may take closer to 9–12 months before full clearance. Recreational athletes—like runners in Aloha or pickleball players in Hillsboro—often return sooner, depending on their sport’s demands.
It’s important to note that even at one year post-op, some athletes still experience calf weakness (10–30% deficits) and reduced endurance. Long-term therapy and maintenance programs are essential for durability.
Conclusion
Rehab after Achilles tendon repair is not a sprint—it’s a carefully staged progression. Each phase builds on the last, from protection and early loading to full sport participation. For athletes and active adults in Hillsboro, Beaverton, and Portland, following this structured path offers the best chance of returning not only to activity, but to confident, pain-free performance.
Whether your goal is hiking the Oregon Coast, running a half marathon, or stepping back on the basketball court, the five-phase rehab framework ensures recovery is safe, steady, and sport-specific. Pain & Performance Coach is the only physical therapy practice in all of the Hillsboro area focused on using the most up to date science to optimize your care and help you reach your performance goals while dealing with an injury.
